







Aromatherapy videos
CHEMOTHERAPY WARNING
Patients should be warned about the dangers of chemotherapy after research showed that cancer drugs are killing up to 50 per cent of patients in some hospitals.
For the first time researchers looked at the numbers of cancer patients who died within 30 days of starting chemotherapy, which indicates that the medication is the cause of death, rather than the cancer.
The study by Public Health England and Cancer Research UK found that across England around 8.4 per cent of patients with lung cancer, and 2.4 per cent of breast cancer patients died within a month.
But in some hospitals the figure was far higher. In Milton Keynes the death rate for lung cancer treatment was 50.9 per cent, although it was based on a very small number of patients.
At Lancashire Teaching Hospitals the 30 day mortality rate was 28 per cent for palliative chemotherapy for lung cancer, which is given when a cure is not expected and treatment given to alleviate symptoms.
Deaths of lung cancer patients from chemotherapy were also far higher than the national average in Blackpool, Coventry, Derby, South Tyneside and Surrey and Sussex, according to the research.
Similarly, around one in five people who underwent palliative care for breast cancer at Cambridge University Hospitals died from their treatment.
Public Health England (PHE), said it had contacted the hospitals concerned to ask them to review practices.
Dr Jem Rashbass, Cancer Lead for PHE, said: “Chemotherapy is a vital part of cancer treatment and is a large reason behind the improved survival rates over last four decades.
“However, it is powerful medication with significant side effects and often getting the balance right on which patients to treat aggressively can be hard.
“Those hospitals whose death rates are outside the expected range have had the findings shared with them and we have asked them to review their practice and data.”
The study looked at more than 23,000 women with breast cancer and nearly 10,000 men with 9634 non-small cell lung cancer who underwent chemotherapy in 2014. Of those treated 1,383 died within 30 days.
Chemotherapy is toxic for the body because it does not discriminate between health and cancerous cells.
The researchers also found that there were significant differences in survival for older people and those in poorer health. They advised doctors to be more careful in selecting patients for treatment where it could do more harm than good.
“The statistics don’t suggest bad practice overall but there are some outliers,” said Professor David Dodwell, Institute of Oncology, St James Hospital, Leeds, UK.
“It could be data problems, and figures skewed because of just a few deaths, but nevertheless it could also be down to problems with clinical practice.
“I think it’s important to make patients aware that there are potentially life threatening downsides to chemotherapy. And doctors should be more careful about who they treat with chemotherapy.”
Professor David Cameron, Edinburgh Cancer Centre, Western General Hospital, Edinburgh, Scotland, added: “The concern is that some of the patients dying within 30 days of being given chemo probably shouldn’t have been given the chemo. But, how many ? There is no easy way to answer that, but perhaps looking at those places/hospitals where the death rate was higher might help.
“Furthermore, if we give less chemo then some patients will die because they didn’t get chemo. It’s a fine balance and the more data we have the better we can be at making sure we get the balance right.”
Professor Peter Johnson, Cancer Research UK’s chief clinician, said: “Chemotherapy is an important part of treatment for many people with cancer. Having information about how well it is being delivered is vitally important to patients and to the health service.”
All the hospitals named said they had since reviewed the cases and were satisfied that chemotherapy prescribing was safe.
The research was published in The Lancet Oncology.







Irridation Formula
The base oil that you use for this treatment is very important. Vegetables oils will do, but much better options are Vinca and Marigold. The Periwinkle, from which Vinca is made, is known to contain certain alkaloids which in some cases can supress the cancerous cells when taken in the form of drugs. If you have the plant in your garden make an infused oil. If you do not have a fresh supply of the periwinkle plant a good herbalist usually has a supply of dried plant matter.
A second option is marigold -infused oil. This shouldn't be Tagetes - The African marigold - but just the humble old garden marigold.
apply the oil once a day to skin that is absolutely clean and dry. Cover the whole torso, including the lower back and abdomen, and pay particular attention to the trauma area. In the case of the uterus, rub well into the tummy; in the case of breast cancer, into the breasts and so on.
Try to start using the oils at least two to three weeks before the irridation treatment is to begin. Sometimes one isn't given an exact date, so start as soon as you are told you are having treatment so that you are prepared even if you are called to the hospital without warning. Don't use it on the days of treatment but use it in-between for at least a month after your last irridation treatment.
| Name | Amount | Dilution | ||
| Lavender | 10 Drops | |||
| Chamomile German | 5 Drops | Dilute in 30mls Vinca infused Oil - or 30mls marigold infused oil | ||
| Chamomile Roman | 5 Drops | |||
| Tagetes | 5 Drops | |||
| Yarrow | 5 Drops | |||
For any loss of hair due to cancer treatment, help can be given by daily massage of the scalp with jojoba oil. When the hair grows again it will be lush and thick.
Treatment with essential oils will not conflict with the treatment given by your doctors. You should not neglect to visit your doctorfor a referral to specialist in the field relevant to your condition. Complementary treatments should be that - complementary.
However, there are many things you can do to help yourself and I would suggest that you get in touch with the Bristol cancer Centre for information on ways to fight cancer with dietary therapy and relaxation methods. This means eating properly and alleviating stress whenever possible. Increase your dose of vitamin C, avoid using commercial chemical body and food preparations, and assume a natural lifestyle as you can manage.
Reference: Fragrant Pharmacy/ V. Wormwood
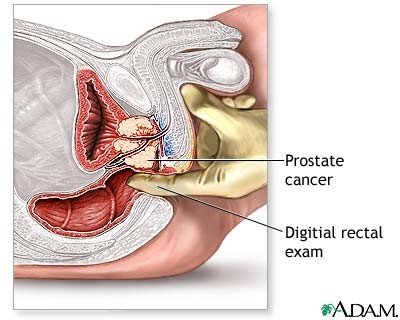
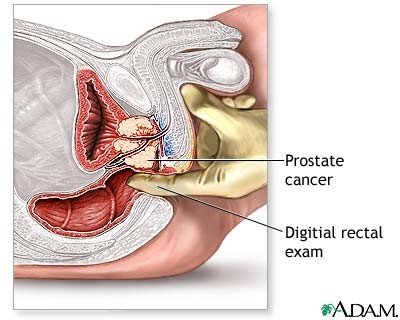
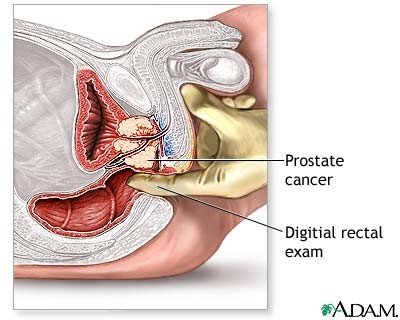
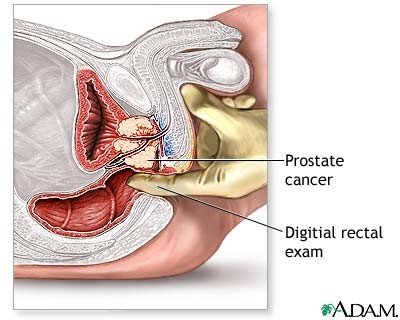
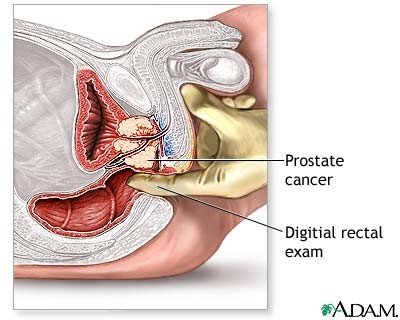
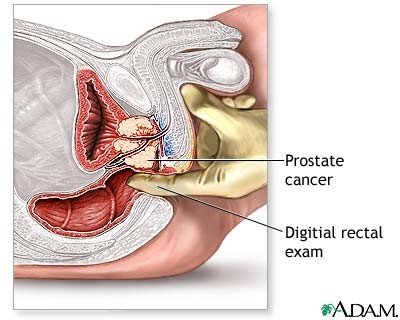
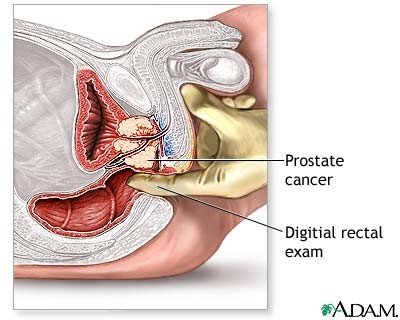
Prostrate Cancer-Radiation Discharge
Your body undergoes many changes when you have radiation treatment for cancer.
You may have the following side effects about 2 to 3 weeks after your first radiation treatment:
⦁ Skin problems. The skin over the treated area may turn red, start to peel, or itch. This is rare.
⦁ Bladder discomfort. You may have to urinate often. It may burn when you urinate. The urge to urinate may be present for a long time. Rarely, you may have loss of bladder control.
⦁ Diarrhea and cramping in your belly, or a sudden need to empty your bowels. These symptoms can last for the duration of therapy. They often go away over time, but some people may have diarrhea flare-ups for years afterwards.
Other effects that develop later may include:
⦁ Problems keeping or getting an erection may occur after prostate radiation therapy. You may not notice this problem until months or even a year or more after therapy is finished.
⦁ Urinary incontinence. You may not develop or notice this problem for several months or years after radiation complete.
Skin Care
A health care provider will draw colored markings on your skin when you have radiation treatment. These markings show where to aim the radiation and must stay in place until your treatments are finished. If the marks come off, tell your provider. DO NOT try to redraw them yourself.
To take care of the treatment area:
⦁ Wash gently with lukewarm water only. DO NOT scrub. Pat your skin dry.
⦁ Ask your provider what soaps, lotions, or ointments are ok to use.
⦁ DO NOT scratch or rub your skin.
Self-care
Drink plenty of liquids. Try to get 8 to 10 glasses of fluids a day. Avoid orange juice, grapefruit juice, and other citrus juices if they make the bowel or bladder symptoms worse.
You can take over-the-counter diarrhea medicine to treat loose stools.
Your provider may place you on a low-residue diet that limits the amount of fiber you eat. You need to eat enough protein and calories to keep your weight up.
Some people who get prostate radiation treatment may begin to feel tired during the time you are having treatments. If you feel tired:
⦁ DO NOT try to do too much in a day. You may not be able to do everything you are used to doing.
⦁ Try to get more sleep at night. Rest during the day when you can.
⦁ Take a few weeks off work or cut back on how much you work.
Intimacy
It is normal to have less interest in sex during and right after radiation treatments end. Your interest in sex is likely to come back after your treatment is over and your life starts to return to normal.
You should be able to enjoy sex safely after radiation treatment is over.
Problems with having an erection are often not seen right away. They may show up or be seen after a year or more.
Follow-up Care
Your provider may check your blood counts regularly, especially if the radiation treatment area on your body is large. At first, you will have PSA blood tests will be checked every 3 to 6 months to check the success of the radiation treatment.
Alternative Names
Radiation - pelvis - discharge
References
D'Amico AV, Crook J, Beard CJ, et al. Radiation therapy for prostate cancer. In: Wein AJ, ed. Campbell-Walsh Urology. 10th ed. Philadelphia, PA: Elsevier Saunders; 2012:chap 104.
Prostate Cancer Treatment (PDQ®) Last Modified: 07/31/2013. Available at: www.cancer.gov/types/prostate/patient/prostate-treatment-pdq. Accessed October 13, 2015
Wilt TJ, MacDonald R, et al. Systematic review: comparative effectiveness and harms of treatments for clinically localized prostate cancer. Ann Intern Med. 2008;148(6):435-48. PMID: 18252677 www.ncbi.nlm.nih.gov/pubmed/18252677.
Zeman EM, Schreiber EC, Tepper, JE. Basics of radiation therapy. In: Niederhuber JE, Armitage JO, Doroshow JH, Kastan MB, Tepper JE, eds. Abeloff's Clinical Oncology. 5th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2014:chap 27.
- Home
- Vaginal infections and inflammation
- Threat to the Forests
- The Vinegar treatment for Thrush
- Treating Acid Environments
- Your Basic Travel Kit - Tummy Troubles
- Pamela L. Crowell on the Prevention and Therapy of Cancer by Dietary Monoterpenes
- Thrush (Candida) Case History
- Problems In Pregnancy
- Thrush treatment for Men- Women
- The Work of Anne-Marie Giraud-Robert
- Fragrant Pharmacy
- Applications For Your Basic Care Kit - 4
- Whooping Cough
- Lymphoedema
- Bites and Stings - General Action - Your Basic Travel Kit
- The journey
- Your Basic Travel Kit - Fevers
- Applications For Your Basic Care Kit - 3
- Aromatherapy-Cramps
- Your Basic Travel Kit - The Heat
- Aromatherapy-Articles-A-Z
- Verrucas and Warts
- Rabid Bites and Scratches - Your Basic Travel Kit
- Your Basic Travel Kit
- Wrinkles and Ageing Skin - Facial Scrubs
- Wrinkles and Ageing Skin - Cleansers
- Wrinkles and the Ageing Skin
- Fragrant way to Beauty - 2
- The Fragrant way to Beauty
- A-Z of Dance and Sports Injuries - 7
- A-Z of Dance and Sports Injuries - 6
- A-Z of Dance and Sports Injuries - 5
- A-Z of Sports and Dance Injuries - 4
- A-Z of Sports and Dance Injuries-3
- A-Z of Sports and Dance Injuries-2
- A-Z of Sports and Dance Injuries
- Aromatherapy - Locker Room Scents
- Aromatherapy- Stress & Sports - Jacuzzis
- Aromatherapy-stress & Sport - Saunas
- Aromatherapy - stress & Sport - Showers
- Stress and Sport - Aromatherapy
- Foot Care - 2 - Aromatherapy
- Foot Care - Aromatherapy
- MUSCLES-Aromatherapy
We have 13 guests and no members online
